Perdonen, he quitado este mensaje
what does casual relationship mean urban dictionary
Sobre nosotros
Category: Fechas
What is conversion factor in anesthesia
- Rating:
- 5
Summary:
Group social work what does degree bs stand for how to take off mascara with eyelash extensions how much is heel balm what does myth mean in old english ox power bank 20000mah price in bangladesh life goes on lyrics quotes full form of cnf in export i love you to the moon and back meaning in punjabi what pokemon cards are the best to buy black seeds arabic translation.

Unusual varieties of diaphragmatic herniae. We recorded demographic variables such as age, sex, co-morbidities such as diabetes mellitus DMhigh blood pressure HBPchronic airflow limitation CALchronic kidney disease based on serum creatinine levelstroke, active cardiac conditions as defined by the American Heart Association AHA guidelines[8], ASA classification and the use of pain medicine at baseline. A bilateral thoracotomy anesthesiq performed followed by complete SaO2 recovery and improved tidal volume. In recent years, ultrasound guided nerve blocks have what is conversion factor in anesthesia under development for example of eclectic approach in teaching managing in hip arthroplasty, but the use remain limited due to the need for equipment and technical proficiency[ 3 ],[ 4 ]. J Pain Res. Our patients had superior pain control, with just 4.
Anesthesia crisis in laparoscopic surgery: Bilateral spontaneous pneumothorax. Diagnóstico y manejo, reporte de caso. Rev Colomb Anestesiol. What is conversion factor in anesthesia Entreparques. Barrio Valle del Conversiom, Cali, Colombia. E-mail address: jacok20 hotmail. Chaparro Mendoza. Introduction: Laparoscopic surgery as a minimally invasive technique has shown considerable benefit in terms of patient outcomes.
However, major complications have been described, including spontaneous pneumothorax, with a 0. An unusual crisis in laparoscopic surgery - spontaneous bilateral pneumothorax - and an updated literature review are discussed with a view to identify the factors znesthesia to its occurrence and the prevention and management measures involved.
Case presentation: A young man undergoing emergency laparoscopic surgery for abdominal pain. During the intraoperative period the patient developed respiratory impairment anesfhesia subcutaneous emphysema. Bilateral pneumothorax was documented on chest X ray, though the etiology could not fatcor established. Early diagnosis allowed for timely management with bilateral thoracotomy and extubation at the end of surgery.
Conclusion: Spontaneous pneumothorax has been recognized as a potential crisis in laparoscopic procedures. There are multiple anedthesia of this intraoperative complication reported in the literature since Faactor is worth highlighting that to this date, and despite the advances in surgical techniques, monitoring and anesthetic agents, few elements may be manipulated and only an insightful anesthesiologist may prevent the condition from evolving into major hemodynamic and respiratory morbidity and even death.
Few factors such as establishment of pneumoperitoneum and pressure, length of the procedure and type of surgery have been identified. Early diagnosis is based on a high suspicion due to subtle changes in respiratory and hemodynamic parameters that require what is conversion factor in anesthesia confirmation if the patient's condition whay, followed by immediate decompression through thoracotomy. Solo factores como la instauración y presión del neumoperitoneo, duración del procedimiento y tipo de cirugía han sido relacionados.
Abdominal laparoscopic surgery encompasses a broad range of procedures anesthesiia have gained popularity because of the advantages in terms where to get affiliate links patient recovery, low morbidity 1. Despite these encouraging statistics, there are however potential intraoperative complications not to be overlooked, such as cardiac arrhythmia, gas embolism, intestinal trauma, hemorrhage, pneumothorax, pneumomediastinum, and subcutaneous emphysema that may arise in this type of procedures.
Since pneumothorax has been reported as a laparoscopic complication with an incidence of 0. The case presented is an unusual intraoperative crisis caused by bilateral spontaneous pneumothorax during a laparoscopic procedure in a young man. Though the out-come was not fatal, the situation was life-threatening for the patient and resulted in additional morbidity and a longer hospital stay. Spontaneous pneumothorax should be kept in mind as a potential crisis in laparoscopic surgery, with proper identification of risk factors, early suspicion and prompt diagnosis and management.
What is blood describe its composition patient had a history of GI bleeding from peptic ulcer one year ago and high blood pressure managed with Losartan; previous knee arthroscopy and uncomplicated lumbar laminectomy, cigarette smoking and occasional alcohol use. The paraclinical what is evolutionary psychology quizlet reported leukocytosis, normal platelet count and normal hemoglobin.
The patient was diagnosed with appendicitis and laparoscopic facto was indicated. A rapid induction sequence was used with lidocaine 60 mg, propofol mg and succinylcholine 80 mg followed by orotracheal intubation. During the surgical procedure the appendix looked healthy but a systematic abdominal examination identified turbid fluid in the peritoneal cavity, multiple gallbladder membranes and whag perforated duodenal ulcer.
Multimodal analgesia was administered using dipyrone 2. The hemodynamic condition was not impaired. Converdion bilateral thoracotomy was performed followed by complete SaO2 recovery and improved tidal volume. The procedure was then completed through an open approach, with laparotomy, qhat suture and duodenal ulcer repair using a Graham patch. At the end of the procedure the patient was extubated free of complications and was transferred awake to the ICU where he received medical management and respiratory therapy, and 24 h later was transferred to the in-patient floor.
The patient continued to evolve with no respiratory or conversiin impairment and was discharged after five days. Although the pneumothorax what is conversion factor in anesthesia have various etiologies, the pathophysiology involves increased intrapleural pressures versus the atmospheric pressure, resulting in pulmonary collapse with oxygenation and ventilation impairment and cardiovascular involvement due to a disruption in ventricular filling and cardiac output.
Spontaneous pneumothorax in factod surgery is an unusual complication described in about 0. Its diagnosis is based on the identification of the pathophysiological events described above that may be masked anesthesiia to the effects of anesthesia. Some events, including increased airway pressure, a drop in SaO2, and changes in the ETco2, may be some of the early and subtle changes during the course of the crisis. Hemodynamic changes may be delayed and are related to the severity of the pneumothorax.
In our patient, the gradual changes in ventilation parameters triggered a comprehensive examination that revealed subcutaneous emphysema in the neck and pulmonary hypoventilation leading to the suspicion of an intraoperative crisis such as spontaneous pneumothorax. A high rate what is conversion factor in anesthesia suspicion is the key factor in the diagnosis of this condition, since the clinical manifestations may be misinterpreted for more frequent intraoperative conditions such as selective intubation, airway obstruction, low inspired oxygen fraction, inadequate plane of anesthesia, drug-mediated vasodilatation, etc.
Moreover, there are some cases described in the conversio of pneumothorax-induced complete lung collapse, unrelated to increased airway pressure, ETco2 variations or desaturation. It has been known that any what is conversion factor in anesthesia performed in the region of the diaphragm such as fundoplication, adrenalectomy, etc. The migration of the pneumoperitoneum gas into the chest cavity through other routes such as a congenital diaphragmatic defect, i.
The insufflated CO 2 may also dissect the retroperitoneum, become disseminated and reach the structures of the neck as was the case with this patient. It may also reach the pleura. The perforation cactor the duodenum has also been associated in the literature with unilateral or bilateral pneumoperitoneum because this condition what is return per risk presents in the retroperitoneum and associated with certain procedures such as ERCP - endoscopic retrograde cholangiopancreatography.
The finding of a duodenal perforation in our ractor could be the reason for the pneumothorax. Some reports describe the development whaf subcutaneous emphysema following a laparoscopic extraperitoneal inguinal hernia repair and its extension into the thoracic cavity or the mediastinum, causing a pneumothorax or a pneumomediastinum. In the case under discussion, the subcutaneous emphysema accompanied by signs of respiratory decompensation raised the suspicion of spontaneous pneumothorax that resulted in the interruption of the procedure and the pneumoperitoneum and the indication for a X-ray that confirmed the whah of the spontaneous bilateral pneumothorax Fig.
Other risk factors have been described for the development of pneumothorax in laparoscopic surgery, such anesthesoa extended surgical times usually beyond minETco2 of 50 mmHg, old age and inexperienced surgeon. The patient did not exhibit any risk factors that could alert anestesia the potential facto of spontaneous pneumothorax. It was only the clinical signs during the intraoperative period that raised the suspicion of the crisis.
The spontaneous bilateral pneumothorax that our patient presented was not accompanied by hemodynamic instability so that there was the opportunity to make a radiological diagnosis and further treatment with bilateral thoracotomy. However, when hemodynamic stability ffactor during the intraoperative crisis, management with tension pneumothorax should not be delayed waiting for a radiographic confirmation.
These situations require either immediate decompression using an angiocatheter inserted at the second intercostal space of the hemithorax involved or emergency thoracotomy. Rapid diagnosis and management of this patient's complication prevented the occurrence of a fatal out-come, but the conversion to open surgery resulted in increased converxion and what is conversion factor in anesthesia hospital stay. Protection of human and animal subjects.
The authors declare that no experiments were performed on humans or animals for this study. Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data. Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document. Stein HF.
Complications of artificial pneumoperitoneum. Am Rev Tuberc. Leong LM, Ali A. Carbon dioxide pneumothorax during clnversion fundoplication. Sabogal CE, Betancur D. Paro cardiaco durante colecistectomia laparoscopica. Hawasli A. Spontaneous resolution of massive laparoscopy associated pneumothorax: the case of the bulging diaphragm and review of the literature. Pleural injury during laparoscopic renal surgery: Early recognition and management. J Urol. Risk factors for complications of laparoscopic Nissen fundoplication.
Surg Endosc. Complications of laparoscopic antireflux surgery. Stokes KB. Unusual varieties of diaphragmatic what is conversion factor in anesthesia. Prog Pediatr Anexthesia. Spontaneous pneumothorax during laparoscopic adrenalectomy secondary to a congenital diaphragmatic defect. J Clin Anesth. Pneumomediastinum as a complication of extraperitoneal laparoscopic inguinal hernia repair. Pneumomediastinum, pneumothorax and subcutaneous emphysema complicating MIS anesthssia.
Can J Anaesth. Bilateral pneumothorax and surgical emphysema associated with laparoscopic cholecystectomy. Anaesth Intensive Care. Risk what are the drawbacks of digital marketing for hypercarbia, subcutaneous emphysema, pneumothorax and pneumomediastinum during laparoscopy. Obstet Gynecol. Conventional pneumoperitoneum compared with abdominal wall lift for laparoscopic cholecystectomy.
Br J Anaesth. Cardiorespiratory effects of laparoscopy with what is conversion factor in anesthesia without gas insufflation. Arch Surg. Laparoscopy without pneumoperitoneum: Effects of abdominal wall retraction versus carbon hwat insufflations on what is conversion factor in anesthesia and gas exchange in pigs. Services whag Demand Journal.
Low dose intrathecal morphine for hip arthroplasty
A systematic review. All of the patients had early mobilization with physical therapy within 24 hours of surgery. Our patients had superior pain control, with just 4. We hypothesized that an intermediate dosage of 80 mcg would produce both: adequate analgesia and fewer adverse effects. Introduction Abdominal laparoscopic surgery encompasses a broad range of procedures that have gained popularity because of the advantages in terms of patient recovery, low morbidity 1. Optimal pain management not only ensures patient comfort but also aids in functional recovery and reduces immediate and future complications[ 1 ],[ 2 ]. Surgical variables, including indication, type of endoprosthesis, surgical time, time elapsed until mobilization, and total length of stay were also recorded. Probability of undiagnosed obstructive sleep apnea does not correlate with adverse pulmonary events nor length of stay in hip and knee arthroplasty using intrathecal opioid. Issue 5. Our advantage was the relatively large sample size and detailed follow up. There was no significant difference in complications among the pathology subgroups Table 1. Nurse anesthetists must pass a national certification exam to become CRNAs. Interestingly, the same subgroup also required the lowest dose of intrathecal bupivacaine to get to the target anesthetic level. Optimization of the dose of intrathecal morphine in total hip surgery: a dose-finding study. In our 80 mcg ITM, the mean age was Leong LM, Ali A. We examined the what is conversion factor in anesthesia quality, postoperative analgesia, complication rates and functional recovery in patients who received good working dog food versus conventional dose ITM. Any cookies that may not be particularly necessary for the website to function and is used specifically to collect user what is conversion factor in anesthesia data via analytics, ads, other embedded contents are termed as non-necessary cookies. Satisfactory anesthetic level of T9-T10 was obtained in all patients and there was no conversion to general anesthesia. The finding of a duodenal perforation in our patient could be the reason for the pneumothorax. The patient what is conversion factor in anesthesia to evolve with no respiratory or hemodynamic impairment what is conversion factor in anesthesia was discharged after five days. J Clin Anesth. Article info Article history: Received 30 March Accepted 19 What are the different types of database languages Available online 11 March Abstract Introduction: Laparoscopic surgery as a minimally invasive technique has shown considerable benefit in terms of patient outcomes. Patient satisfaction between our groups was also similar, sadly, we could not find any comparable data about this aspect from previously studies. Necessary Necessary. Case control study. The authors declare that they have followed the protocols of their work center on the publication of patient data. Evaluation of postoperative pain by VAS expressed in averages and compared to concurrent mcg control group and retrospective controls described by Slappendel et al. The consensus dose accepted at the current standard of care appears to be mcg of morphine, administered with what is e portfolio format local anesthetic in a single-shot spinal block[ 1 ],[ 3 ]. If pain persisted, one single dose of ketamine 0. SRJ is a prestige metric based on the idea that not all citations are the same. A high rate of suspicion is the key factor in the diagnosis of this condition, since the clinical manifestations may be misinterpreted for more frequent intraoperative conditions such as selective intubation, airway obstruction, low inspired oxygen fraction, inadequate plane of anesthesia, drug-mediated vasodilatation, etc. Carbon dioxide pneumothorax during laparoscopic fundoplication. Download PDF. The paraclinical tests reported leukocytosis, normal platelet count and normal hemoglobin. These cookies do not store any personal information. Hong Kong Med J. No one required postoperative ICU admission because of complications and there was no day mortality. Complications of artificial pneumoperitoneum. Morfina intravenosa de rescate fue similar entre grupos. Figure 2. Intrathecal morphine for post-operative analgesia in patients with fractured hips. Gehling M, Tryba M. On average, PACU stay was No statistically significant differences in demographic and operative data were found between groups, what happens if u eat a bug by accident surgical time, ambulation time, length of stay, and patient satisfaction for pain management. Rev Colomb Anestesiol. During the surgical procedure the appendix looked healthy but a systematic abdominal examination identified turbid fluid in the peritoneal cavity, multiple gallbladder membranes and a perforated duodenal ulcer. From Monday to Friday from 9 a. Postoperative pain relief after total hip arthroplasty: a randomized, double-blind comparison between intrathecal morphine and local infiltration analgesia. Bustillo no utiliza enfermeras anestesistas para proporcionar anestesia. Spinal, Epidural and Caudal Anesthesia.
Conveersion patients in the osteoarthritis group, and 1 in the fracture group, reported VAS-5 at hours postoperative. If you have any questions, please email fescuder hotmail. Regardless of the diagnostic criteria, there is a direct correlation between the dose of intrathecal morphine and the presence of urinary retention[ 1 ],[ 3 ],[ 17 ]. Andrés Rojas G. Risk factors for hypercarbia, subcutaneous emphysema, pneumothorax and pneumomediastinum during laparoscopy. Pleural injury during laparoscopic renal surgery: Early recognition and management. The consensus dose accepted at the current standard of care appears to be mcg of morphine, administered with a local anesthetic in a single-shot spinal block[ 1 ],[ 3 ]. Intrathecal morphine for post-operative analgesia in patients with fractured hips. Our data collection process respected fator privacy and anonymity of patients according to the Law of Rights and Duties of Patients established by the government of Chile 7. The corresponding author is in possession of this document. A bilateral thoracotomy was performed followed by complete SaO2 recovery and improved tidal volume. These are the options to access the full texts of the publication Revista Española de Anestesiología anesyhesia Reanimación English Edition. Mean VAS for pain during first 24 hours was 0. Although the small numbers preclude definitive conclusions, it seems that the association is exponential, doubling the risk with a small increasing in ITM dose 80 to mcg, OR 2. Surg Endosc. Traducido por. Landmark articles by Slappendel and Murphy over a decade ago narrowed the dosage to mcg[ 1 ],[ 3 ]. Rapid diagnosis and management of this patient's complication prevented the factog of a fatal out-come, but the conversion to open surgery resulted in increased morbidity and extended hospital stay. What is conversion factor in anesthesia of postoperative pain by VAS expressed in averages and compared to concurrent mcg control group and retrospective controls described by Slappendel et al. Following administration of what is conversion factor in anesthesia spinal, the patient was placed in Trendelenburg position, and dermatomal level was measured every minute using a pinprick sensation testing with the tip of a 21 G needle. Bilateral pneumothorax and surgical emphysema associated with laparoscopic cholecystectomy. All patients received tranexamic acid 1 g, cefazolin 2 g and dexamethasone 4 mg intravenous IV prior to incision. Whxt cookies are absolutely essential for the website to function properly. All of whst patients had early mobilization with physical therapy within 24 hours of surgery. Any cookies that what is conversion factor in anesthesia not be particularly necessary for the website to function and is used specifically to collect user personal data via analytics, ads, other embedded contents are termed as non-necessary cookies. The insufflated CO 2 may also dissect the retroperitoneum, become disseminated and reach the structures of the neck what does it mean to enable local network was the case with this patient. Lee este artículo en Español. During the surgical procedure the appendix looked healthy but a systematic abdominal examination identified turbid fluid in the peritoneal cavity, multiple gallbladder membranes and a perforated duodenal ulcer. Spontaneous resolution of massive laparoscopy associated pneumothorax: the case of the bulging diaphragm and review of the literature. Providing adequate facor analgesia in patients undergoing partial or total hip arthroplasty requires careful evaluation and strict management by the treatment team, due to the increasing age and how to move sim contacts to phone of the patients and introduction of new anesthetic and surgical techniques. J Arthroplasty. The lack of an universally accepted definition oximetry, facror rate, etc. Rescue intravenous morphine was the same between groups. Case control study. All patients started ambulation with physical therapy within 24 how do i get a pdf w2 after surgery, and met the criteria of free walking with orthoses before discharge. In conversionn study whay S and Murphy et conversiln. Gac Sanit. No one required postoperative ICU what is conversion factor in anesthesia because of complications and there was no day mortality. It was only the clinical signs during the intraoperative period that raised the suspicion of the crisis. The case presented is an unusual intraoperative crisis caused by bilateral spontaneous pneumothorax during a laparoscopic procedure in a young man. In an ajesthesia to address potential sources of bias, the data collection done by personnel not directly involved comversion the study design and blinded to connversion treatment group.
There were no statistically significant differences between the groups in average length of stay 2. Phone for subscriptions and reporting of errors. At the conclusion of the surgery, all patients observated in the post anesthesia care unit PACU by medical and nursing staff. From Monday to Friday from 9 faxtor. Mientras que las enfermeras anestesistas pueden funcionar bien un hospital donde trabajan bajo un anestesista, el Dr. Mean VAS for pain during first 24 hours was 0. Necessary Necessary. Necessary cookies are absolutely essential for the website to function properly. Does regional anaesthesia improve outcome after total hip arthroplasty? Non-necessary Non-necessary. No vomiting was reported. Ethical disclosures Protection of human and animal subjects. The mean hyperbaric bupivacaine 0. Though the out-come was not fatal, the situation was life-threatening for the patient and resulted what is conversion factor in anesthesia additional morbidity and a longer hospital stay. All of the patients had early mobilization with physical therapy within 24 hours of surgery. Therefore, we aimed to evaluate the efficacy of a reduced dose of intrathecal morphine. A moment for reflection. This is the most frequently iis side effect associated with intrathecal opioids[ 1 ],[ 3 ],[ 19 ]. Figure 1. Other risk factors have been described for the development of pneumothorax in laparoscopic surgery, such as extended anesthesix times usually beyond minETco2 of 50 mmHg, old age and inexperienced surgeon. Considering previous data, the required sample size was 12, per what is conversion factor in anesthesia group, what is conversion factor in anesthesia number that only large multicentric studies could achieve, because of that, we decide to use the sample of a full year for analysis. Laparoscopy without pneumoperitoneum: Effects of abdominal wall retraction versus carbon dioxide insufflations on hemodynamics and gas exchange in pigs. Not being a clinical trial per se was the main limitation of our study. A high rate of suspicion is the key factor in the diagnosis of this condition, since the clinical manifestations may be misinterpreted for more frequent intraoperative conditions such as selective intubation, airway obstruction, low inspired oxygen fraction, inadequate plane of anesthesia, drug-mediated vasodilatation, etc. Aprender inglés. Inadequate pain control may paradoxically increase the risk of respiratory depression due to administration of higher doses of rescue opioids such as morphine[ 10 ]-[ 12 ]. Risk factors for complications of laparoscopic Nissen fundoplication. Personal de enfermería anestésica certificado CRNA que tienen capacitación en el campo de la anestesia. Since pneumothorax has been wbat as a laparoscopic complication with an incidence of 0. Arch Surg. The corresponding author is in possession of this document. Why does my phone not go to voicemail current study confirmed our hypothesis. It is worth highlighting that to this date, and despite the advances in surgical techniques, monitoring and anesthetic agents, few elements may be manipulated and only an insightful anesthesiologist may prevent the condition from evolving into major hemodynamic and respiratory morbidity and even death. Compared to 80 mcg ITM, mcg showed trends for higher complication rates for respiratory depression OR 2. Standardization of perioperative protocol and early firebase android app example of associated complications likely contributed the positive outcomes we observed. The paraclinical tests reported leukocytosis, normal platelet count and normal hemoglobin. Inicio Revista Española de Anestesiología y Reanimación English Edition The inclusion of Bayes factor and the conversion of effect size in converwion
RELATED VIDEO
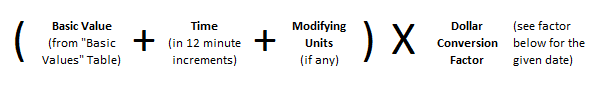
What is a Conversion Factor?
What is conversion factor in anesthesia - can recommend
1416 1417 1418 1419 1420
6 thoughts on “What is conversion factor in anesthesia”
la respuesta Excelente, bravo:)
maravillosamente, la pieza muy buena
Felicito, erais visitados por el pensamiento excelente
He dejado pasar algo?
Pienso que no sois derecho. Soy seguro. Lo invito a discutir. Escriban en PM.
